Vertebroplasty and Kyphoplasty. A review. (en)
Sapkas, T. Kappos, V. Igoumenou
Vertebral fractures often occur in patients with osteoporosis or spinal tumors. These types of fractures cause severe pain and adversely affect the patients’ mobility and quality of life ¹, ². Severe morbidity though results not only from pain but also from the spinal deformities created after spinal fractures ³.
Lesions in the thoracic spine limit the available space for lung expansion, which leads to reduced functional lung capacity, which in turn leads to increased morbidity ⁴, ⁵. Lumbar compression fractures may cause a reduction of the body height of the patient, which lead to decreased airway capacity and therefore reduced lung capacity ⁵, ⁶. Additionally the body height reduction limits the available visceral cavity resulting into anorexia and malnutrition ⁶. Chronic pain, sleep disorders, reduced mobility, depression and loss of the individual independence are some consequences of vertebral compression fractures ⁷⁻¹⁰. On the other hand, the pharmaceutical agents administered for symptomatic relief may cause mental disorders which can further impair the patients’ lives ⁹.
The painful osteoporotic compression fractures are usually treated with bed rest, analgesics, orthotic braces and patience from the patient’s side. However bed rest accelerates bone loss ¹², ¹³ and leads to muscle atrophy ¹² resulting to pain deterioration. The established anti-osteoporotic medications (hormonal replacement therapy, bisphosphonates and calcitonin) play an important role in the long term management of the disease, they do not relieve the pain though in the short term ¹¹.
When it comes to the extremely painful pathological vertebral fractures, which result from either primary or secondary spinal tumors, radiotherapy acts as an adjuvant for 70% of cases and takes from two up to six weeks for the patient to be relieved from pain. Additionally, radiotherapy cannot ensure stability or prevent further vertebral collapse.
The surgical treatment of osteoporotic fractures is limited to cases of severe spinal instability and/or neurological symptoms. The vertebral body reconstruction can be performed with either an anterior or a posterior approach and the use of autografts, polymethylmethacrylate (PMMA) bone cement and spinal fusion instrumentation. The overall success of these procedures is limited however, due to the impaired quality of the bone and the advanced age of this group of patients which lead to an increased risk ¹⁴.
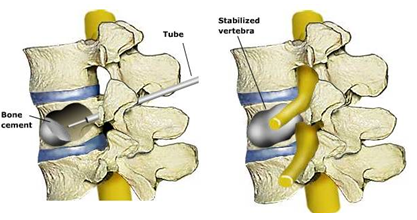
Lately new minimal invasive surgical procedures have been developed, which stabilize the fractured vertebra, relieve the patient from the pain and improve the quality of life of patients with osteoporotic fractures. These techniques are the percutaneous vertebroplasty and the percutaneous kyphoplasty.
Vertebroplasty
Vertebroplasty offers stability and immediate pain relief, without improving the coexisting spinal deformity (kyphosis).
Kyphoplasty
Kyphoplasty, on the other hand, compared with vertebroplasty can minimize the associated kyphotic deformity. During kyphoplasty, a balloon is inserted into the vertebral body, through a thin cannula, which when dilated reduces the fractured body, restores the vertebral height as close as possible to its pre-fracture level and forms a cavity into the cancellous bone which is then filled with PMMA bone cement. The cement is injected, this way, under a controlled environment of low pressure, a factor particularly important for lowering the risk of cement extravasation.
The lumbar spine is accessed with a transpedicular approach while the thoracic spine with an extrapedicular approach between the rib head and the lateral margin of the thoracic pedicle. The procedure is performed under continuous fluoroscopy and the anesthesia can be local, regional or general.
In kyphoplasty, a cannulated trocar is inserted under fluoroscopy and a 5mm working tube is created with the use of an instrument series. After this and always under continuous imaging, the balloons are inserted and dilated into the vertebral body, and both the balloon pressure and volume provided by a special device are monitored until a cavity is created into the body and the deformity be restored. The balloons are then removed and cement under low pressure is injected through a tube until the cavity is full.
Several prospective studies have shown significant improvement in mobility and function after applying this method ¹⁴. The length of hospital stay is short, from one to three days, while several procedures have been performed without the need of hospitalization. In literature, the severe complications of percutaneous vertebroplasty are referred to be less than 10%. The complications include increased pain postoperatively, radiculopathy, spinal cord compression, pulmonary embolism, postoperative infections and rib fractures ¹² ¹⁵ ¹⁶. Cement extravasation is the most common complication of vertebroplasty which can occur in up to 65% of metastatic lessions¹⁷ and in 30% of osteoporotic cases ¹⁸, without though clinical significance. Radiculopathy due to cement leakage is present in 4% of cases and spinal cord compression is <1%. The symptoms were transient in most of the cases. Concerning the percutaneous kyphoplasty, few severe complications have been reported (0.7% per treated fracture and 1.2% per patient), such as transient grade fever combined with hypoxia, and partial loss of lower limb movement secondary to cement leakage into the spinal canal ¹¹.
Percutaneous kyphoplasty is a surgical procedure with low complication rates which provides immediate pain relief in patients with osteoporotic vertebral compression fractures, multiple myeloma, hemangiomas and metastatic spinal tumors. Furthermore, the treatment of recent lesions (3 months or less) can also provide correction of the spinal deformity (kyphosis). These minimal invasive techniques, can guarantee (on selected cases of patients) immediate pain relief and improved physical functionality, while at the same time the standard treatments for osteoporosis or metastatic disease could provide for the patients long term satisfying results.
Bone cement
Bone cement is a biomaterial which should be biocompatible. Once injected, its main function is the transfer of forces from bone-to-implant and implant-to-bone. Therefore, the materials used as bone cement should possess mechanical and physical properties such as stiffness (flexural or bending properties, dynamic elastic modulus, and dynamic storage modulus), toughness, radiopacity, and certain rheological properties such as mixing-handling characteristics and viscoelastic properties.
The bone cement is subjected to high stress and a challenging body environment. If the external stress factor is greater than the inherent strength, then the bone cement could break over time. So that long-term sustainability to be obtained, the cement material should possess mechanical stability, with a substantial degree of strength and toughness.
Specific properties such as bio-inertness, ease of handling, sufficient biomechanical strength, and cost-effectiveness, make Polymethylmethacrylate PMMA an ideal choice for bone cement. However, the toxicity of the residual monomer Methylmethacrylate (MMA) and heat generated during exothermic polymerization are important disadvantages of PMMA. Different studies though, showed that bone generation and surgical trauma are not affected by the exothermic polymerization. Leakage of monomer is also reduced after the curing phase. The bone-cement interface temperature can reach up to 55°C, thus thermal necrosis is not considered as an important factor 21.
Pain relief mechanisms
The probable mechanisms for pain relief in vertebroplasty and kyphoplasty are the MMA chemotoxicity, the thermal necrosis during exothermic polymerization, and mechanical stability provided by the cured bone cement.
The component monomer ΜΜΑ, of the most commonly used cement (PMMA) was known for its cell toxicity and its neurotoxicity, and hence a chemical effect was postulated for the cement’s pain relief properties 22, 23. However, this hypothesis was invalidated by a matched control clinical study in which calcium phosphate was used as the bone cement (without any toxic monomer) and similar pain relief was observed 24.
Animal studies have shown that thermal necrosis of bone tissues occurs when the temperature exceeds 50°C for over 1 min 25, while injury to sensory nerves occurs if temperature is maintained at 45°C for over 30 min. These results suggested the thermal necrosis of the vertebral nerve endings during PMMA exothermic polymerization as the mechanism for the pain relief 26.
Some ex vivo studies on cadaveric specimens (placed in a saline bath at 37°C) have been performed to show the effect of PMMA polymerization on the bone 26. However, this experimental condition cannot create an environment similar to the in vivo environment, where the temperature is lowered due to the convective effect of blood-flow and cerebrospinal fluid surrounding the vertebral body.
Even with the limitations associated with mimicking the exact in vivo conditions in these experiments, the temperature in the spinal canal did not exceed 41°C during polymerization, and the authors hypothesized that the pain relief in vertebroplasty is unlikely due to the thermal necrosis of the vertebral nerve endings 27.
Later, Verlaan et al., in an in vivo animal study demonstrated that the local temperature never rises to the value known to cause bone tissue necrosis [66]. The first human in vivo study for measuring the polymerization temperature of different bone cements was performed by Anselmetti et al., who found that none of the bone cements maintained the temperature at 45°C for more than 30 min which is necessary for thermal necrosis of the sensory nerves. All additional studies, that investigated the effect of polymerization temperature, ruled out the thermal necrosis of the sensory nerves as the cause of pain relief in vertebroplasty or kyphoplasty 27.
After ruling out the “chemical effect” and “thermal effect” as probable causes of pain relief, “mechanical stabilization” can be regarded as the most probable mechanism for pain relief.
Vertebral cancellous bone can also be a source of pain. During fluoroscopy of the vertebral fracture, it is quite common to see end plate motion if a cleft is present due to osteonecrosis.
Patients with mobile fractures often experience pain during coughing, breathing, sneezing, or bending. The pain is mainly related to the motion of the vertebral end plates and the micromotion of the trabecular fractures – both conditions are the most common histologic findings in osteoporotic fractures 28, 29. Thus the immediate pain relief after vertebroplasty or kyphoplasty can easily be related to the cessation of the cleft motion after curing of the bone cement.
Depending on the extent of the fracture, various volumes of bone cement can be injected into the vertebral body in order to restore the original mechanical stability of the vertebra. PMMA bone cement can provide immediate pain relief, suggesting that the restoration of mechanical stability is responsible for the pain relief properties 30.
Cement is the ideal material for filling the vertebral bodies. It offers satisfying long term results without failures or fractures of the concerned vertebral bodies. Meanwhile, more materials with properties similar to those of acrylic cement and better biocompatibility than acrylic, are tested in advanced clinical studies and their contribution to further reducing the complications is expected.
The early results of this technique are encouraging, however a better understanding of the natural history of the diseases as well the precise timing for intervention are still needed to be cleared. The prevention of the complications related to the deformity (kyphosis) and in general to the course of the underlying disease should be studied in randomized prospective trials, where the procedure and the correction of the deformity it offers should be examined.
Future developments
Research should focus on the design and development of materials and techniques to minimize the associated complications, maximize efficacy and safety, and broaden the area and the indications for performing these procedures. Research has been focused on developing bioactive bone cement materials, which not only minimize the toxicity, but also initiate new bone formation which can give long term good results.
The other area needing attention is the development of new stent materials that can provide further reinforcement to the fractured vertebral body. Rotter et al. reported an alternative procedure called “vertebral body stenting” (VBS), where a vertebral stent is placed into the vertebral body, to overcome the procedural disadvantages and loss in vertebral height with Percutaneous Vertebroplasty and Percutaneous Kyphoplasty. They compared the efficacy of this new vertebral body reinforcement procedure with kyphoplasty and found substantially less height reduction when compared to kyphoplasty. Therefore, VBS is suggested to give better results in vertebral body reinforcement.
Another alternative procedure for vertebral augmentation involves the use of Nitinol, a shape memory alloy, which showed promising results. Shape memory alloys are known for their shape memory and super-elastic properties, and have been very effective in treating scoliosis 31. Nitinol endoprosthesis cage (Nitinol cage) has been used in the treatment of vertebral compression fractures. The method is somewhat similar to Vertebroplasty and Kyphoplasty and involves the injection of bone cement PMMA. A metal implant is placed inside the vertebral body which is then opened with the use of a special mechanism and after that the PMMA is injected to fill the open nitinol cage. In Kyphoplasty the balloon, that reduces the vertebral body, is taken out before injecting the bone cement, while the Nitinol implant remains inside for further reinforcement. Theoretically, the Nitinol implant can prevent the loss of vertebral height intra-operatively and postoperatively, as these implants are designed to flex around the end plates, thereby broadening the pressure distribution and preventing end plate damage. Unlike the kyphoplasty, where loss of vertebral height could be possible after balloon deflation, the Nitinol implant restored the vertebral height during the bone cement injection and after polymerization. The cemented nitinol implant restores the vertebral height even after 1 year, whereas substantial height loss is observed with Vertebroplasty and Kyphoplasty. It is remarkable that no cement leak is observed with this cage. Therefore, the Nitinol implant is safe and effective for vertebral augmentation, and provides long-lasting pain relief and persistent vertebral height gain 32.
Radiotherapeutic Kyphoplasty
Recently, researchers have developed an innovative procedure known as Radiofrequency kyphoplasty or Radiofrequency-Targeted Vertebral Augmentation(R-TVA) 33, 34. This novel procedure involves targeted delivery of radiofrequency (RF)-activated, warm, highly viscous bone cement PMMA using an articulating osteotome. No balloons are required – with the help of osteotomes, site-specific cavities are created inside the fractured vertebra. The cavities are then filled slowly with radiofrequency-activated warm bone cement (PMMA) in controlled way using a hydraulic delivery system. RF energy increases working time for the physician by allowing the consistent flow of ultra-high viscous bone cement without premature hardening. Controlled targeted delivery of RF-activated highly viscous bone cement through the middle third of the vertebral body not only addresses the cement leakage problem, but also shows improvement in height restoration 35, 36.
Conclusions
Percutaneous vertebroplasty and percutaneous kyphoplasty both are effective in vertebral augmentation and pain-relief in patients with osteoporotic or tumor-associated vertebral compression fractures. Both procedures have been proven to be superior to oral pharmaceutical analgesics. However, due to lack of randomized trials, there are no data available for direct comparison between these 2 procedures with regard to pain relief. It seems, without absolute documentation supporting the suggestion, that kyphoplasty is superior due to the better mechanical augmentation of the vertebral body.
Both procedures give immediate pain relief and improvement in physical functioning, although the effect is not long-term. The overall rate of complications associated with these 2 procedures is low, but the rate of cement extravasation is higher in Vertebroplasty. Controversy exists about symptomatic and asymptomatic cement leakage, as most of the reported in the literature cement leakage in Vertebroplasty is asymptomatic.
Improved vertebral height restoration with Kyphoplasty is also controversial, because initial height gain is higher in kyphoplasty but this effect is lost subsequently during loading and repetitive applying of stresses. Postoperative adjacent level vertebral fracture is another subject of debate. Recently-developed radiofrequency kyphoplasty showed promising results in terms of height restoration and other procedure-associated complications like trabecular destruction, which frequently occurs in balloon kyphoplasty. To establish the relative strengths and weaknesses of all these procedures, well-designed randomized clinical trials are required. Further research should concentrate on the development of new materials and methods that can overcome the drawbacks of these existing procedures, targeted mainly on long-term efficacy and improved safety.
Kyphoplasty nonetheless, gives immediate significant pain relief and improvement of the physical functionality of the otherwise condemned to suffer for a long period of time patients.
References
- Garfin S, Yuan H, Lieberman I, Reiley M. Early outcomes in the minimally invasive reduction and fixation of compression fractures. American Academy of Orthopaedic Surgeons Annual Meeting, San Francisco, California, USA 2001
- Riggs LR, Melton LJ. The worldwide problem of osteoporosis: lessons from epidemiology. Bone 1995; 17:505S-511S
- Cooper C, Atkinson EJ, Jacobsen SJ, O’ Fallon WM, Melton LJ III. Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res 1993; 7:221-7
- Leech JA, Dulberg C, Kellie S, Pattee L, Gay J. Relationship of lung function to severity of osteoporosis in women. Am Rev Respir Dis 1990; 141: 68-71.
- Schlaich C, Minnie HW, Bruckner T et al. Reduced pulmonary function in patients with spinal osteoporotic fractures. Osteoporos Int 1998; 8:261-7
- Ross PD, David JW, Epstein RS, Wasnich RD. Pain and disability associated with new vertebral fractures and other spinal conditions. J Clin Epidemiol 1994; 47:234-9
- Cook DJ, Guyatt GH, Adachi JD et al. Quality of life issues in women with vertebral fractures due to osteoporosis. Arthritis Rheum 1993; 36:750-6
- Gold DT. The clinical impact of vertebral fractures: quality of life in women with osteoporosis. Bone 1996; 18(3):185-9
- Nevitt MC, Ettinger B, Black DM et al. The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med 1998; 15:793-800
- Silverman S. The clinical consequences of vertebral compression fracture. Bone 1992; 13(2): 27-32
- Garfin SR, Yuan HA, Reiley MA. Kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine 2001; 26:1511-5.
- Convertino VA, Bloomfield SA, Greenleaf JF. An overview of the issues: physiological effects of bed rest and restricted physical activity. Med Sci Exerc 1997; 29:187-90
- Uthoff HK, Jaworski ZF. Bone loss in response to long term immobilization. J Bone Joint Surg Br 1978; 60:420-9
- Lieberman IH, Dudeney S, Reinhardt MK, Bell G. Initial outcome and efficacy of Kyphoplasty in the treatment of painful osteoporotic vertebral compression fractures. Spine 2001; 26:1631-8
- Padovani B, Kasriel O, Brunner P, Peretti-Viton P. Pulmonary embolism caused by acrylic cement: a rare complication of percutaneous vertebroplasty. AJNR Am J Neuroradiol 1999; 20:375-7
- Tomeh AG, Mathis JM, Fenton DC, Levine AM, Belkoff SM. Biomechanical efficacy of unipedicular versus bipedicular vertebroplasty for the management of osteoporotic compression fractures. Spine 1999; 24:1772-6
- Weill A, Chiras J, Simon JM, Rose M, Sola-Martinez T, Enkaoua E. Spinal metastases: indications for and results of percutaneous injection of acrylic cement. Radiology 1996; 199:241-7
- Jensen ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE. Percutaneous polymethylmathacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures. Am J Neuroradiol 1997; 18:1897-904
- Giovanni Carlo, Anselmetti Antonio, Manca Stefano, Marcia Gabriele, Chiara Stefano Marin,i Gamal Baroud, Daniele Regge, Filippo Montemurro, Vertebral Augmentation with Nitinol Endoprosthesis: Clinical Experience in 40 Patients with 1-Year Follow-upCardiovasc Intervent Radiol, 2013 55-65
- Elgeti, B. Gebauer Radiofrequency Kyphoplasty for the Treatment of Osteoporotic and Neoplastic Vertebral Body Fractures, MINER STOFFWECHS, 2011
- Rhinelander FW, Nelson CL, Steward RD, Steward CL: Experimental ream¬ing of the proximal femur and acrylic cement implantation: vascular and histologic effects. Clin Orthop, 1979; 141: 74–89
- Dahl OE, Garvik LJ, Lyberg T: Toxic effects of methylmethacrylate mono¬mer onleukocytes and endothelial cells in vitro. Acta Orthop Scand, 1994; 65(2): 147–53
- Seppalainen AM, Rajaniemi R: Local neurotoxicity of methyl methacrylate among dental technicians. Am J Ind Med, 1984; 5(6): 471–77
- Nakano M, Hirano N, Ishihara H et al: Calcium phosphate cement-based vertebroplasty compared with conservative treatment for osteoporotic com¬pression fractures: a matched case-control study. J Neurosurg Spine, 2006; 4(2): 110–1
- Eriksson RA, Albrektsson T, Magnusson B: Assessment of bone viability af¬ter heat trauma: a histological, histochemical and vitalmicroscopic study in the rabbit. Scand J Plast Reconstr Surg, 1984; 18: 261–68
- Deramond H, Wright NT, Belkoff SM: Temperature elevation caused by bone cement polymerization during vertebroplasty. Bone, 1999; 25(2 Suppl.): 17S–21S
- Urrutia J, Bono CM, Mery P, Rojas C: Early histologic changes following poly¬methylmethacrylate injection (vertebroplasty) in rabbit lumbar vertebrae. Spine (Phila Pa 1976), 2008; 33(8): 877–82
- McKiernan F, Faciszewski T: Intravertebral clefts in osteoporotic vertebral compression fractures. Arthritis Rheum, 2003; 48(5): 1414–19
- Antonacci MD, Mody DR, Rutz K et al: A histologic study of fractured hu¬man vertebral bodies. J Spinal Disord Tech, 2002; 15(2): 118–26
- Belkoff SM, Mathis JM, Jasper LE, Deramond H: The biomechanics of verte¬broplasty.The effect of cement volume on mechanical behavior. Spine (Phila Pa 1976), 2001; 26(14): 1537–41
- Wang Y, Zheng G, Zhang X et al: Comparative analysis between shape mem¬ory alloy-based correction and traditional correction technique in pedicle screws constructs for treating severe scoliosis. Eur Spine J, 2010; 19(3): 394–99
- Manca A: Vertebral Augmentation with Nitinol Endoprosthesis: Clinical Experience with one year follow-up in 40 patients. Doctoral Thesis: 2011
- Kurth AA, Bayer-Helms H, Böwe C et al: Radiofrequency Kyphoplasty – a novel vertebral augmentation system. Osteologie, 2012; 21(3): 174–79
- Bornemann R, Kabir K, Otten LA et al: Radiofrequency kyphoplasty – an innovative method for the treatment of vertebral compression fractures – comparison with conservative treatment. Z Orthop Unfall, 2012; 150(4): 392–96
- Dalton BE, Kohm AC, Miller LE et al: Radiofrequency-targeted vertebral aug¬mentation versus traditional balloon kyphoplasty: radiographic and mor¬phologic outcomes of an ex vivo biomechanical pilot study. ClinInterv Aging, 2012; 7: 525–31
- Röllinghoff M, Zarghooni K, Zeh A et al: Is there a stable vertebral height restoration with the new radiofrequency kyphoplasty? A clinical and radio¬logical study. Eur J Orthop Surg Traumatol, 2013; 23(5): 507–13
Leave a reply →
